The evaluation of risks and benefits is essential in medicine. In radiology, this is reflected in the application of the principles of justification and optimization. Consequently, proper radiological practice must necessarily consider the simultaneous quantitative assessment of the risks and benefits involved. In diagnostic imaging, various approaches have been developed to estimate the risk induced in the patient by the use of ionizing radiation. On the other hand, there are currently no methods to quantify the benefit of a radiological investigation. As a consequence, it is impossible to perform a comprehensive, objective, and quantitative justification and optimization of radiological practices.
The main obstacle to the quantitative description of risks and benefits in radiology is the inability to characterize them using comparable units. A possible approach to overcome this issue is to assess the benefit also in terms of risk. By following this approach, the lack of benefit for the patient associated with an incorrect diagnosis can represent the so-called clinical risk associated with the radiological procedure.
In the study published in Nature Communications Medicine, for the first time, a mathematical model was developed to define the total risk of a radiological procedure by considering both radiation risk and clinical risk. Such a total risk was characterized as a function of radiation risk, the prevalence of the examined disease, the false positive to true positive ratio, the life expectancy loss associated with an incorrect diagnosis, and the interpretive performance of radiologists in terms of area under the ROC curve (AUC). This model was applied to a population of one million virtual twins simulating a clinical scenario for the investigation of liver cancer. The virtual twins were generated to be representative of the U.S.A. population in terms of sex, age, race/ethnicity, and anatomical dimensions.
The study revealed that, across all demographic groups clinical risk exceeded radiation risk by at least four times. Moreover, in 90% of cases, optimization based on the application of the introduced mathematical model would have resulted in a reduction of the total risk only by increasing the associated radiation dose. The risk-to-benefit ratio of a radiological procedure can be characterized in a risk versus risk framework by calculating both radiation risk and the associated clinical risk using comparable units. This approach allows for a quantitative and holistic approach to the justification and optimization of diagnostic imaging exams. The results highlighted how, in modern radiology, it is possible to consider cases where a radiation dose increase can be associated with a benefit for the patient and that, in some cases, an extreme and unjustified radiation dose reduction can compromise the diagnosis and even harm patients.
Francesco Ria
Carl E. Ravin Advanced Imaging Labs, Center for Virtual Imaging Trials
Department of Radiology, Duke University Health System,Durham, NC, USA
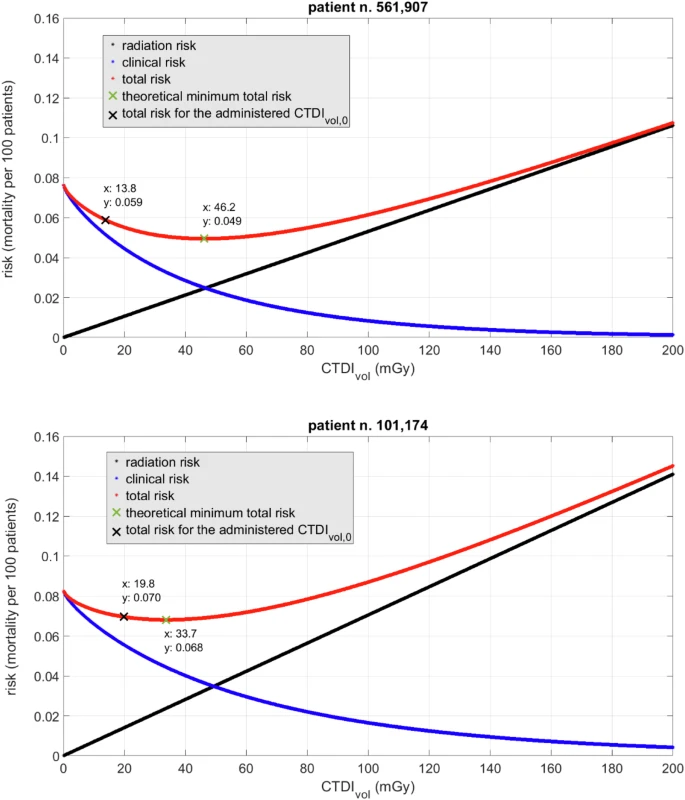
Patient examples
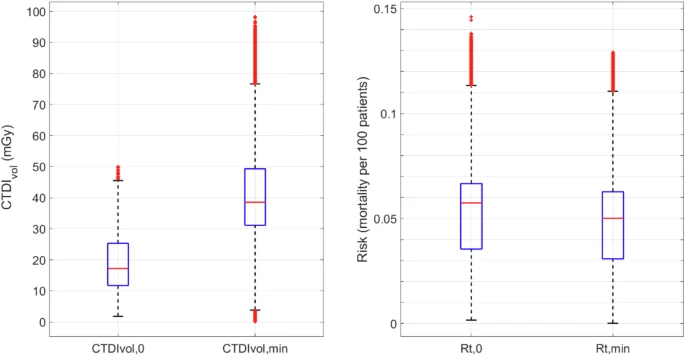
Scanner output and total risk comparisons
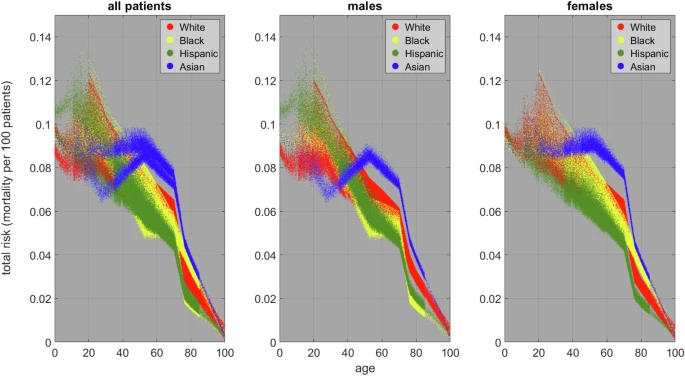
Minimum total risk


